Wednesday, July 22, 2020
In my last post three weeks ago I observed the trend that the number of new daily COVID-19 cases had been increasing for two months in LA County while deaths from COVID had been decreasing. That post generated many questions and responses. (Thanks!) Today I’d like to update us on the situation in LA and answer some of the questions you posed.
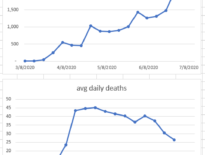
About two weeks ago death rates reversed their previous declines and rose to a seven-day average in the mid-40s, which is where they were back in April. (See the graphs above.) Forty-something deaths per day in a county of ten million people might not seem like a lot, but the usual annual mortality in LA County is 60,000. Forty deaths a day amounts to a quarter of that total and is about the same as the number of deaths from the greatest killer in LA County – heart disease. So a sustained rate of 40 deaths daily would be awful.
In the last two weeks hospitalizations for COVID have climbed and have reached new highs. I should make it clear that we are not in immediate danger of running out of hospital beds, but the trend is clearly in the wrong direction. And of course the number of new daily COVID cases continue their rise, now tallying more than 3,000 new cases per day.
So my hypothesis in my last post that low risk individuals were increasingly exposed to COVID while high risk individuals were effectively protecting themselves clearly failed. Apparently as the number of new infections continued to grow, they were not limited to those who would easily recover. In that post I suggested that we shift our focus from figuring out the sorts of establishments that can reopen to instead figuring out the sorts of people who can safely go to any establishment. But that suggestion depends on death rates declining, so it’s moot for now. And, in fact, last week the Governor ordered many businesses that had reopened, like gyms, hair salons and malls, to reclose.
Let me turn now to some of your questions.
Shouldn’t even people at low-risk continue to wear face coverings and practice physical distancing?
Absolutely, and I should have said so explicitly in my last post. Now that death rates are climbing, we should all stay home when possible. When we venture outside, we should maintain distance from others and wear face coverings. And everyone should wash their hands frequently.
There are some suggestions that COVID infection has long-term consequences. Isn’t that a reason that even people at low risk take strict precautions?
To be clear, now that death rates are high, everyone should take strict precautions. Whether low-risk people can be more lax is a question to take up when death rates are low again. There is some evidence that some patients have protracted injuries to their lungs, brains, and hearts months after COVID infection. The frequency and magnitude of these complications are unclear, however. Recall that many people with COVID have no symptoms (and presumably no organ injury) at all. Whether these injuries resolve or persist in the long term won’t be known until the long term. But the unclear possibility of harm in the distant future does not seem like the sort of risk that would generate consensus about closing businesses. We don’t close bars even though we understand the long-term risks of drinking alcohol. We closed businesses to keep our hospitals from being immediately flooded with patients, not to prevent health consequences years from now.
High-risk patients don’t live in a cocoon. By necessity they interact with others even if only to pursue essentials, like medications and groceries. Since those others might be at low risk, doesn’t that mean that all of us must act as if we’re at high-risk to protect those who are?
Maybe. And if so, then my suggestion last time is unworkable. If low-risk people can’t segregate with only other low-risk people, then high-risk people will necessarily be harmed as case counts rise. And this may be exactly what happened two weeks ago. If at some prevalence of disease the infection will always “leak” out of the low-risk silo and into the high-risk silo, then we can’t afford to let the case counts rise. It would be nice if that wasn’t the case. It would be nice to let low-risk people get on with their lives, generate income, and reform frayed social ties if they could do so without consequence to their health or to others’ health. That would result in case counts continuing to rise while death counts remained stable or declined.
But that isn’t what’s happening. So until things improve, each of us has to stay away from others, wear a face covering, and wash our hands, as if we’re the only one keeping our neighbor, our relative, our grocer, or our pharmacist out of the hospital. Because we might be.
Learn more:
Newsom orders statewide reclosures (LA Times, July 13)
As 13 New Deaths and 2,593 New Cases of COVID-19 are Confirmed, Revised Health Officer Order Requires Closure of Additional Indoor Operations and Sectors: Actions come as Public Health releases new K-12 protocol to provide “roadmap” to help schools plan for reopening (News Release July 13, LA County Dept of Public Health)
Majority of Newly Reported COVID-19 Cases are in People Under 41 Years Old, New High of COVID-19 Hospitalizations – 11 New Deaths and 2,848 New Cases of Confirmed COVID-19 in Los Angeles County (News Release July 19, LA County Dept of Public Health)
COVID-19 page (LA County Dept of Public Health)
My previous posts about the pandemic:
Summary, Speculation, Suggestion (July 3)
Think Local, Act Local (April 27)
Testing, Testing Part 2 (April 17)
Of Masks And Meaningful Measures (April 5)
Updates From The Socially Distant (March 30)
Testing, Testing (March 26)
Novel Coronavirus FAQ Part 2 – Pandemic Hullabaloo (March 20)
Coronavirus Frequently Asked Questions (March 13)
Community Transmission Of Novel Coronavirus In LA County (March 11)
What You Need To Know About The Novel Coronavirus (March 1)